Why The Challenge Initiative and Evidence-based Strategies for Family Planning Matter More Than Ever
The Challenge Initiative (TCI) is a global platform that supports cities and local governments to rapidly and sustainably scale up proven primary health care solutions, particularly family planning. Rather than introducing new or parallel interventions, TCI transfers evidence-based strategies that are already known to work and supports local governments in institutionalizing these approaches within their own systems. By strengthening leadership, management, and data use at the local level, TCI achieves strong results at scale while promoting long-term sustainability. At a time of shrinking global health funding, this direction offers exceptional value for money—protecting past gains while enabling countries to expand impact with fewer external resources.
The year 2025 marked a challenging transition for TCI with its project completion. For country teams, including ours in the Philippines, 2025 raised critical questions about continuity, expectations, and sustainability. How would momentum be sustained? What would the next phase demand in terms of focus and capacity? And how could gains in family planning and adolescent, youth, and sexual and reproductive health be protected amid tighter global financing?
These questions were very much present as I travelled to Senegal to attend the TCI Global Chief of Party Meeting. There was a strong need for clarity on strategic direction, operating models, and performance expectations. Like many colleagues from other hubs, we arrived seeking reassurance and a clearer understanding of how TCI would move forward.

What the meeting ultimately provided was a shared perspective. Listening to the experiences of other hubs across Africa and Asia made it clear that the Philippines was not alone in navigating uncertainty. Many teams had faced similar transitions, pressures, and doubts. At the same time, they shared stories of adaptation, resilience, and continued impact. This collective reflection helped normalize the challenges of the past year and reinforced a shared sense of purpose across the global TCI community.
The discussions were grounded in realism. TCI is operating in a global environment where development assistance for health is increasingly constrained, making efficiency and focus more critical than ever. The meeting acknowledged these realities openly, including leaner global support structures and the need for greater hub-level autonomy. Importantly, this shift was framed not as a setback, but as an evolution toward a more mature and sustainable operating model.
For the Philippines, this message resonated strongly. Over the past years, TCI, in partnership with the Zuellig Family Foundation, has demonstrated its role as a powerful scale-up engine, enabling cities to rapidly expand access to modern family planning services using proven approaches. By working through local governments, TCI strengthens health systems, builds institutional capacity, and embeds data-driven decision-making where it matters most. These are not short-term wins, but foundational improvements designed to endure beyond external support.
This is precisely why TCI matters now more than ever. In a context of shrinking global health budgets, TCI’s model delivers high impact at relatively low cost. By leveraging existing systems, local leadership, and tested practices, TCI maximizes return on investment while reducing long-term dependence on donor funding. It protects what has already been achieved and enables countries to do more with less.
The global meeting reinforced this value proposition. Despite the uncertainties experienced in 2025, the collective results from the NextGen phase demonstrate TCI’s credibility and global reach. Across multiple countries, TCI-supported cities have reached millions of women with family planning services, contributing to healthier families and stronger communities. These results are measurable, well documented, and replicable across diverse contexts.
Encouragingly, the meeting also brought clarity and optimism about the future. Continued funding from Bayer, alongside ongoing discussions with other partners, signals sustained confidence in TCI’s approach. While resource mobilization remains a shared responsibility, the opportunity ahead is clear. TCI offers a compelling platform for donors seeking efficient, scalable, and sustainable investments in primary health care and family planning.
For our team in the Philippines, the meeting was both affirming and energizing. It validated the strategic direction we are taking under TCI 20.30, with an emphasis on prioritization, operational efficiency, and strong local ownership. Approaches such as clustered city support, streamlined reporting, and practical, on-demand access to knowledge at the facility level align well with the global push to simplify systems while safeguarding results.
Leaving the meeting, the uncertainty that characterized much of 2025 gave way to clarity, reassurance, and confidence. TCI is entering its next phase not as an untested initiative, but as a proven mechanism for translating global evidence into local impact. For governments, partners, and donors committed to advancing primary health care and family planning, TCI represents an opportunity to protect past investments and scale what works in a way that is efficient, locally led, and built to last.
Author: Dr. Anthony Faraon, ZFF TCI-Philippines Chief of Party
TCI-Philippines Draws Lessons from Indonesia’s Family Planning Landscape
The Indonesia landscaping workshop last December 2025, in partnership with Jalin Foundation and supported by The Challenge Initiative (TCI)-Philippines and global colleagues, offered a rare glimpse into a country with a rich family planning (FP) history and a health system in active transition. Designed to help local partners prepare for the launch of the new TCI Indonesia Hub, the workshop surfaced valuable insights about Indonesia’s strengths, complexities, and emerging opportunities for impact.
A Strong National FP Foundation
Indonesia’s national FP program reflects decades of progress and remains one of the strongest in the region. The 2024 Family Data Update highlights a modern contraceptive prevalence rate (mCPR) of 62.38% among married women, alongside a stable method mix dominated by injectables and pills, with gradual growth in implants and IUDs. These indicators demonstrate a solid foundation on which cities and districts can continue expanding FP access and strengthening quality of care.
A notable structural feature is that these indicators apply only to married women, as public facilities provide FP services exclusively to married clients. Adolescents and unmarried women typically rely on private providers and pay out of pocket—a big difference from the Philippine context, where FP services in public facilities are universally available regardless of marital status.
City-Level Diversity as an Opportunity
Beneath Indonesia’s strong national picture lies significant variation across cities, not as weaknesses, but as opportunities for more tailored, context-driven strategies. mCPR among married women ranges from 37.9% in Central Jakarta to 61.2% in Bandung, while unmet need* ranges from 16.0% to 35.0%. Several cities are already surpassing national targets for long-acting reversible contraceptives (LARC) uptake, while others show steady upward trajectories.
This diversity underscores the value of localized action plans and city-led decision-making—precisely the environment where TCI’s coaching approach can help accelerate progress.
Urban Realities: A Unique Set of Challenges and Strengths
Indonesia’s cities present a mix of robust service platforms and distinct implementation challenges. With more than 53,000 FP service points, the country benefits from wide availability of services. A unique feature is the strong presence of independent midwife practices, which provide FP services to 36.46% of married women, a larger share than in the Philippines, where public health centers are the primary FP providers.
Workshop discussions highlighted several key opportunities for Indonesia’s cities:
- Supporting FP method continuation in fast-paced urban environments.
- Strengthening counselling and side-effect management to reduce switching and discontinuation of FP methods.
- Enhancing postpartum FP, especially given the country’s high postpartum visit coverage (77.63% nationally).
These are natural challenges in any large, diverse urban setting—the very challenges that TCI aims to help cities address through practical tools, coaching, and evidence-based interventions.
A Decentralized System With Parallels, and Distinctive Features
Indonesia, like the Philippines, operates a decentralized governance system where districts and cities oversee FP implementation. The two countries share common experiences related to varying local priorities, the importance of local champions, and the need for strong coordination across sectors.
However, Indonesia’s system also has distinct characteristics, including:
- Centralized procurement of FP commodities handled by BKKBN (Badan Kependudukan dan Keluarga Berencana Nasional, “National Population and Family Planning Board”), ensuring national-level consistency in supply.
- Implementation led by district and city health offices, creating a clear division between national procurement and local service delivery.
- Strong community-based cadres, such as the TPK (Tim Pendamping Keluarga, “Family Support Team”), who play an active role in family development and outreach.
These features shape Indonesia’s FP landscape in unique ways and offer a clear structure for where TCI support can add value.
FP at the Center of Human Capital Development
One of Indonesia’s strongest assets is its ability to position FP within a broader development vision. Under BKKBN’s 2025–2029 Transformation Priorities, FP is deeply connected to:
- reducing stunting,
- supporting youth development,
- strengthening family resilience,
- driving digital innovation through tools like SIGA (Sistem Informasi Keluarga, “Family Information System”), and
- advancing community-based behavior change.
This framing aligns FP with Indonesia’s long-term human capital goals, creating a powerful foundation for TCI to build upon as it supports cities in designing integrated, family-centered FP strategies.

Looking Ahead
The workshop revealed a country that is not only committed to FP, but also fully prepared to take its next strategic leap. Indonesia’s strong policy environment, extensive service delivery platforms, and energized local actors create an ideal landscape for the establishment of the TCI Indonesia Hub.
The momentum is clear: city leaders, local health offices, community cadres, and national counterparts all demonstrate readiness to adopt practical, and scalable approaches. With TCI’s coaching support, Indonesia is well-positioned to accelerate the translation of national priorities into city-level results, particularly in expanding choice, improving service quality, and reaching underserved urban populations.
* Unmet need refers to the proportion of women of reproductive age who want to delay or stop childbearing but are not using any method of contraception.
Author: Dr. Anthony Faraon, ZFF TCI-Philippines Chief of Party
Reflections on Strengthening Local Leadership and Governance Practice
Serving as a panelist for two institutions undergoing Performance Governance System (PGS) assessments—the Local Government Unit (LGU) of Limay and Navotas City Hospital (NavCH)—offered me a rare vantage point into how governance, when taken seriously, becomes a living system that shapes culture, performance, and ultimately, the well-being of communities. These experiences, grounded in the work of the Institute for Solidarity in Asia (ISA), provided valuable insights that deeply align with the health governance principles we advance in the Zuellig Family Foundation (ZFF). They affirmed a central truth: governance is essential, and there is a replicable system that helps leaders translate aspirations into measurable progress.
Leadership Ownership as the Foundation
One of the most striking observations from both Limay and NavCH was the strong ownership shown by senior leaders. In Limay, the mayor and department heads demonstrated not only familiarity with their strategies but also a commitment to embedding these into the LGU’s day-to-day governance. In NavCH, the hospital director and management team exhibited similar dedication—an understanding that achieving proficiency under PGS is not merely a compliance exercise but a strategic shift in how the institution envisions its role in delivering quality health services.
This leadership ownership is not symbolic; it is operational. At both institutions, strategies were cascaded down to staff, creating alignment across units and ensuring that the work of frontline personnel was directly tied to broader institutional goals. This echoes one of ZFF’s long-held principles: transformation happens when leaders champion the change and empower others to carry the vision.
The Power of Multisectoral Engagement
Both Limay and NavCH demonstrated the value of multisectoral councils—a core requirement of the PGS. These councils provided governance structures with breadth and diversity, enabling a wider range of stakeholders to co-own the institution’s goals. The councils asked thoughtful questions, brought in external perspectives, and reinforced transparency and accountability.
For ZFF, this reinforces what we have long practiced in our Health Leadership and Governance Program (HLGP): sustainable health outcomes require whole-of-community engagement. The PGS experience affirms that multisectoral structures remain essential—not as peripheral advisory bodies but as strategic partners in steering direction and sustaining momentum.
Integration: A Natural Area for Strengthening

In both Limay and NavCH, one area that emerged as part of their ongoing governance journey is the need to further harmonize the many strategies, programs, and performance requirements that institutions must manage. This is not a shortcoming; rather, it is a common reality for dynamic organizations operating in complex environments. As priorities expand and new mandates are introduced, institutions are continually challenged to ensure that their strategies remain coherent and mutually reinforcing.
Similarly, the refinement of outcome measurement continues to evolve. Both institutions have already established solid foundations for tracking progress, and they are now at the stage of sharpening how these metrics can more clearly reflect the quality and impact of their work. This is a natural progression—moving from counting activities to capturing meaningful changes in the lives of the people they serve.
These insights resonate with what we observe in our work at ZFF: institutions that are growing and maturing often reach a point where aligning strategies and deepening measurement become opportunities for greater clarity and acceleration. Rather than obstacles, they signal that an organization is ready to move to the next level of governance practice.
What This Means for ZFF’s Work
My experience as a panelist affirms that the PGS model has elements that are highly relevant to ZFF’s approach to health governance. Several insights stand out:
- A structured governance framework accelerates transformation. The discipline of strategy maps, scorecards, and accountability mechanisms strengthens institutions’ ability to operationalize reforms—a lesson ZFF can integrate more deliberately in helping LGUs sustain health systems improvements.
- Cascading strategies to frontline workers must be intentional. Just as PGS requires, ZFF can encourage LGUs and health facilities to ensure that midwives, nurses, barangay health workers, and administrative staff all understand how their roles contribute to health outcomes.
- Multisectoral bodies must evolve from being consultative to being strategic partners. The PGS Governance Council offers a model for how ZFF-supported local health boards and local health teams can deepen their engagement, shift from compliance to stewardship, and anchor decisions on evidence.
- Measurement should be simplifiable and meaningful. ZFF’s metrics for health leadership and systems development can benefit from the PGS discipline of focusing on indicators that truly reflect progress and impact.
A Replicable System for Better Governance
What makes the PGS experience compelling is its replicability. While the contexts of Limay and NavCH differ, both institutions benefited from a governance system that is structured, strategic, and grounded in accountability. For ZFF, this reinforces our core belief that effective governance is not accidental—it is built, practiced, and continually refined.
As we continue working with LGUs and health facilities across the country, integrating these insights can help strengthen our approach and deepen the impact of our leadership and systems development programs. The PGS experience is a reminder that governance is not only possible, but transformative, when leaders embrace a clear system and commit to sustaining it.
Photos from: ISA
Author: Dr. Anthony Faraon, ZFF The Challenge Initiative-Philippines Chief of Party
Leading from the Future: Reflections from the International Conference on Family Planning
When our team boarded the flight to Bogotá for the 2025 The Challenge Initiative (TCI) Annual Meeting and the International Conference on Family Planning (ICFP), we carried more than presentations and data sets. We carried the stories of 24 Philippine cities that have chosen to lead boldly in family planning (FP) and adolescent sexual and reproductive health (ASRH). As a relatively young hub in the global TCI network, the Philippines has always been both a learner and a contributor. This year, however, felt different. For the first time, we arrived not merely to listen but to help shape the direction of the Initiative.
Related articles:
- Nine Cities Recognized as Global Self-Reliant Cities in Reproductive Health
- Eight Cities Share Success in Family Planning and Adolescent Health
A Gathering Shaped by Urgency and Imagination
The theme of the Annual Meeting, “Lead from the Future,” captured the spirit of the meeting. Representatives from six TCI hubs across 13 countries came together, each navigating shrinking donor resources, political transitions, and data challenges. Yet despite these pressures, the mood was determined and forward-looking.
In his opening message, TCI Executive Director Kojo Lokko reminded us that the Initiative’s evolution—from Good to Great and Growth Mindset to Reaching New Heights—has always pointed toward long-term sustainability. Leading from the future, he explained, requires clarity about what we hope to achieve and the discipline to act today in ways that bring that vision closer to reality.
Listening to him, I saw how closely this reflects the Philippine journey. In five years, we moved from launching a hub at the height of a lockdown to establishing governance, leadership development, data use, and sustainable financing as the backbone of city programs. Our experience has been a constant cycle of learning, adapting, and improving—often under constraints but always grounded in the belief that cities can lead the change themselves.
Local Leadership at the Center
Our delegation brought this story to the global stage through five scientific presentations at ICFP and through the voices of two city partners: Dr. Benson Panaguiton, City Health Officer of Dipolog City, and Judith Catalan Janiola, City Population Officer of General Santos (GenSan) City.
Judith’s presentation on GenSan’s experience captured attention. She described how local leaders use data not only to monitor performance but also to solve problems, realign priorities, and motivate teams. She highlighted practical actions driven by partnerships with youth organizations, faith leaders, barangay officials, and civil society groups. These efforts helped reduce teenage pregnancies and strengthened community ownership.
A Shifting Global Landscape
Across sessions—from Bayer’s keynote to discussions on domestic financing—a consistent message emerged: the global environment for FP is changing rapidly. Donor funding is tighter, pronatalist and anti-rights movements are gaining momentum, and climate disruptions are affecting service delivery. Health systems must now be more resilient, adaptable, and grounded in local ownership.
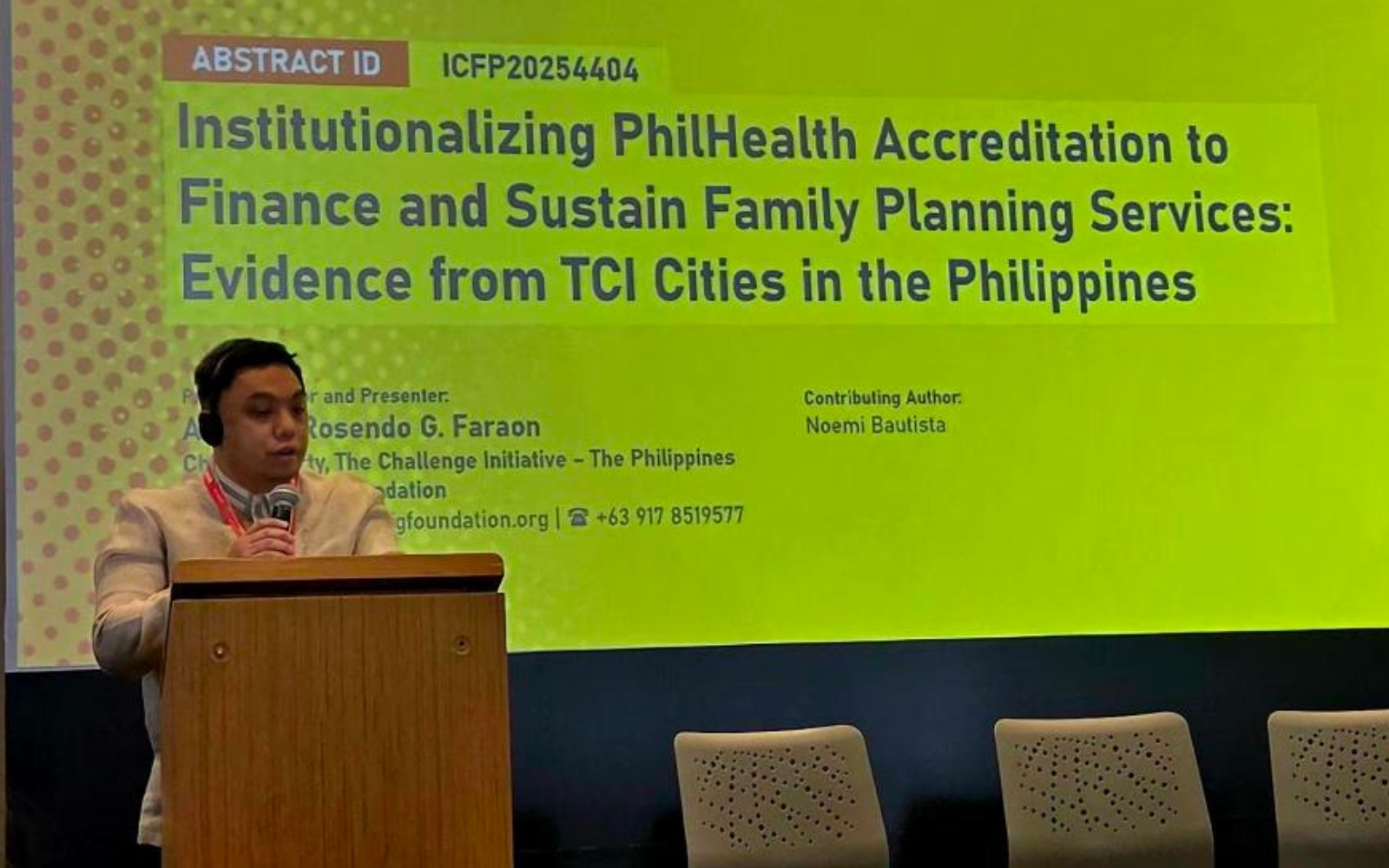
During a flash-oral presentation, I shared how Philippine cities are beginning to tap PhilHealth reimbursements to finance FP services. This drew interest, especially from teams exploring sustainable financing models. The idea that a national insurance system can support FP programs illustrates the potential of strengthening and fully utilizing local systems.
Our Monitoring, Evaluation, and Learning Manager, John David, also shared how standardized data presentations transformed city leadership meetings. Data became easier to understand and discuss, encouraging more leaders—from mayors to youth representatives—to use evidence as the basis for decisions.
Expanding the Philippine Contribution Through Posters
The delegation also presented three posters highlighting how TCI-Philippines strengthens city systems:
- Deputy Chief of Party Pamela Mangilin showcased the Leadership for Adolescent and Youth-Friendly Cities (LAYFC) youth engagement model, demonstrating how trained young leaders create safe spaces and support adolescent reproductive health.
- City Team Leader Teresa Ferrolino presented how inclusive leadership, multisector collaboration, and community involvement enable cities to integrate FP and ASRH into development plans.
- John David examined inconsistencies between local and national FP data and recommended improvements in data governance.
Collectively, these posters highlighted how the Philippine hub advances youth leadership, governance, and data quality to support sustainable FP programs.

Leading From the Future in the Philippine Context
Some of the most meaningful exchanges happened outside formal sessions. Colleagues from other countries asked how a small Philippine team expanded to 24 cities while maintaining cost-efficiency. They inquired about City Leadership Teams, budget protection, and governance reforms aligned with national systems.
These conversations confirmed that the Philippines is becoming a source of global learning. Our strength lies in combining leadership development, system integration, and practical governance tools—elements that help cities continue performing even in uncertain environments.
To lead from the future in the Philippine context means focusing on what works: building strong leaders, institutionalizing coaching and onboarding, optimizing PhilHealth financing, integrating routine data use, partnering with youth and communities, and preparing FP systems to withstand political and environmental change. It means trusting local governments to lead while providing the right support and accountability mechanisms.
A Future Already Emerging
As our delegation left Bogotá, I felt a renewed sense of direction. The future that TCI envisions is already visible in Dipolog, General Santos, Iligan, and across the other 21 partner cities. These local governments are proving that FP does not survive because of projects; it thrives because leaders take responsibility for it.
Author: Dr. Anthony Faraon, ZFF TCI-Philippines Chief of Party
Mandaue City’s Path Toward Sustainable Family Planning and Adolescent Health
The Zuellig Family Foundation, through its The Challenge Initiative (TCI)-Philippines team, met with Mandaue City Mayor Thadeo Jovito “Jonkie” Ouano, City Health Officer Dr. Debra Maria Catulong, and the dedicated staff of the City Health Office. The discussion highlighted the city’s steady progress in advancing family planning and adolescent health services over the past two years, while also laying out a shared vision to sustain and build on these gains in the years to come.
Bringing Services Closer to Families
When Mandaue City first joined TCI in 2023, access to family planning was limited. Only five midwives in the entire city had the skills to provide certain contraceptive services, and residents often had to travel far or wait for schedules to receive care. Today, that situation has been transformed. All 27 barangay health centers now have trained midwives, nurses, and doctors who can provide modern contraceptives on a daily basis.
This decentralization of services has had a direct impact on families. The city’s modern contraceptive prevalence rate has risen from 19 percent in 2020 to 30 percent in 2024—meeting the national target. Behind these numbers are women who are better able to space their pregnancies, parents who can provide for their families with greater stability, and adolescents who can make informed choices about their futures.
Related articles:
- Mandaue City Redefines Reproductive Care through Women’s Health Caravan
- Eight Cities Share Success in Family Planning and Adolescent Health
Making Services Adolescent-Friendly
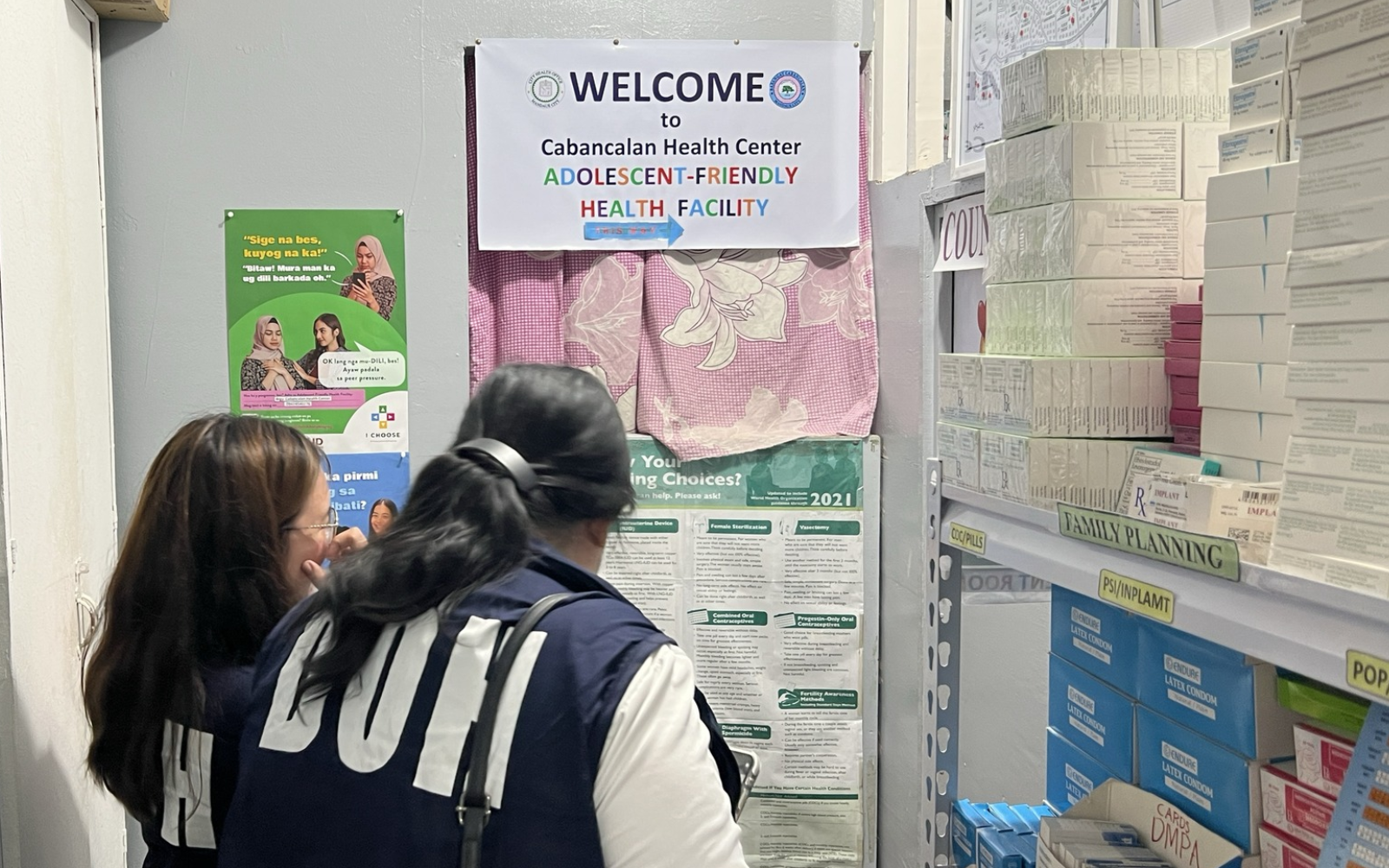
The city also recognized early on that adolescents face distinct barriers when seeking health services. Young people often hesitate to ask for help because of stigma or fear of being judged. To address this, Mandaue invested in adolescent-friendly health services (AFHS), redesigning facilities to ensure privacy and training staff to listen and respond without judgment.
As of today, ten barangays have already achieved certification from the Department of Health as adolescent-friendly, and the rest are moving toward the same goal. With these changes, adolescents in Mandaue are finding spaces where they feel welcome, safe, and respected.
Integrating Family Planning into Everyday Care
A significant innovation in Mandaue has been the integration of family planning into the full range of health activities. Whether through immunization drives, cancer screenings, or women’s health check-ups, family planning has become part of routine care. This approach helps normalize conversations about reproductive health and ensures that no opportunity is missed to provide information and services.
Investing in Sustainability
The city has also demonstrated strong political and financial commitment. From 2.5 million pesos in 2024, the budget for family planning and adolescent health rose to 12 million pesos in 2025—a fivefold increase. This reflects both the prioritization of reproductive health and the recognition of its importance in improving overall well-being.
At the same time, Mandaue is pursuing PhilHealth accreditation for its facilities and providers. This will allow reimbursements to flow back into the health system, creating a financial cycle that sustains services over time. Coupled with the Special Health Fund under Universal Health Care, the city is positioning itself for long-term continuity of family planning and adolescent health programs.
Key Lessons from Mandaue’s Experience
Several lessons stand out from Mandaue City’s journey. Strong local leadership, led by the mayor and supported by the city council, has been central to accelerating reforms. Systems change is possible when local governments commit to decentralization, integration, and youth-friendly service delivery. Listening to adolescents and families has helped ensure that services are relevant and stigma-free. Finally, financial sustainability must be built deliberately, as demonstrated by the city’s budget increases and its pursuit of PhilHealth reimbursements.
Looking Ahead
Despite these successes, challenges remain. The city aims to achieve adolescent-friendly certification across all barangays, expand peer education networks, and continue strengthening data quality and use. Ensuring a consistent supply of commodities and fully utilizing available budgets will also be critical to sustaining progress.
What is most notable is the sense of ownership within Mandaue City. Local leaders, health workers, and communities see these programs not as external projects but as their own responsibility. This perspective is the clearest sign that sustainability is within reach.
Mandaue City’s story is one of determination, innovation, and leadership. From expanding access to family planning, to creating youth-friendly spaces, to embedding sustainability through financing, the city has demonstrated how local governments can drive meaningful health reforms.
By making services more accessible to families and more welcoming to adolescents, Mandaue is showing what it means to build a healthier and more empowered community. Its experience serves as a model for other cities in the Philippines—and beyond—on how to combine political will, systems strengthening, and community-centered design to achieve lasting impact.
Meeting photos from: Mandaue City Public Affairs Office
Author: Dr. Anthony Faraon, ZFF TCI-Philippines Chief of Party
Lapu-Lapu City’s Path to Strengthening Family Planning and Adolescent Health
On September 18, 2025, the Zuellig Family Foundation, through its The Challenge Initiative (TCI)-Philippines team, met with the Lapu-Lapu City government to discuss family planning and adolescent health. Joining the meeting were City Administrator Atty. Almendras and the City Health Office team, led by nurses Ivy Amistad, Jovy Alonzo, and Leizel Lagtapon. The conversation served as a chance to reflect on the city’s progress, identify ongoing challenges, and consider ways to strengthen impact and sustainability.
Recovery and Resilience after COVID-19
Like many local government units, Lapu-Lapu City experienced major disruptions in reproductive health services during the COVID-19 pandemic. Health workers were diverted to pandemic response, service delivery slowed, and demand for family planning dropped. Now, the City is steadily regaining momentum. With health staff back on the ground, there has been recovery in the uptake of short-acting methods such as pills, injectables, and condoms. Encouragingly, long-acting and permanent methods (LAPMs) like implants, intrauterine devices (IUDs), and sterilization are also increasing in demand.
One area where Lapu-Lapu has exceeded expectations is in postpartum family planning (PPFP). Through sustained training and outreach activities, the city has exceeded its TCI commitment of ensuring that targeted providers are trained on PPFP–demonstrating that with political will and operational focus, service delivery can quickly regain strength.
Related article:
Addressing the Data Gap
Reliable data is critical for decision-making, yet the city continues to face difficulties in capturing a complete picture of family planning performance. Public facilities generally provide regular reports, though private birthing centers and hospitals show variable compliance rates. An ordinance requires reporting, but enforcement is limited without established legal penalties. The City Health Office is considering connecting compliance requirements to business permit processes and incorporating maternal death review procedures as accountability measures.
Another challenge lies in the transition to new Department of Health (DOH) performance indicators. Health staff are still adjusting from measuring modern contraceptive prevalence rate (mCPR) to tracking “demand satisfied”, which looks at the percentage of women with demand for family planning and who are actually using modern methods. Lapu-Lapu currently reports a demand satisfied rate of only 46%, far below the 70% national target. Continued coaching and capacity building will be essential to ensure that data is not only accurate but also used strategically for planning and advocacy.
Investing in Young People
Adolescent health remains a priority in Lapu-Lapu. Several health workers have been trained on adolescent-friendly health services (AFHS), and facilities are starting to offer confidential, youth-centered care. While formal DOH accreditation is still in development for most facilities, efforts are underway to address infrastructure needs, including the establishment of appropriate counseling spaces.
Despite these challenges, peer education is emerging as a promising practice. By mobilizing young people themselves to reach their peers, the city is creating more relatable and effective pathways to information and services. Plans are underway to expand peer education networks through collaboration with the Sangguniang Kabataan (SK) Federation and barangay-level initiatives. For sustainability, the city will need to determine the right peer-to-population ratio to ensure meaningful coverage across communities.
Governance, Financing, and Sustainability
Lapu-Lapu has demonstrated strong commitment to financing reproductive health, earmarking four million pesos in 2024 and five million pesos in 2025 for FP and adolescent health.
Budget execution has been gradual, with 22% of funds utilized by mid 2025, indicating opportunities to accelerate implementation timelines to maintain program momentum. This highlights the potential for strengthening alignment between program objectives and financial planning. For example, advancing demand satisfied rates from 46% to 60% would involve specific resource requirements for peer educators, supplies, and community outreach activities, each with defined costs. Developing such costing frameworks could support city leadership, including the mayor and city council, in making strategic resource allocation decisions for optimal program impact.
In May 2025, the City completed a self-reliance assessment using TCI’s Reflection and Action to Improve Self-reliance and Effectiveness (RAISE) Tool. The results showed strong performance in data management (100%) and leadership (85%). However, areas needing improvement include formalizing policies, ensuring specific line-item allocations for FP and adolescent health, and strengthening supportive supervision systems. These gaps highlight where technical assistance and local leadership need to converge to ensure sustainability.
Moving Ahead
The meeting underscored both the progress and the unfinished work in Lapu-Lapu City’s reproductive health journey. On the one hand, the city has demonstrated resilience, ownership, and momentum—recovering service delivery, expanding postpartum FP, and investing in adolescent-friendly health services. On the other hand, challenges remain: persistent gaps in data reporting, budget execution, and demand satisfied rates reveal the need for stronger systems and sharper strategies.
With committed leadership, available resources, and the support of partners like ZFF and TCI, Lapu-Lapu City is well-positioned to transform these challenges into breakthroughs. By enforcing policies, scaling up peer-led youth programs, and aligning financial investments with program outcomes, the city can not only close its current gaps but also emerge as a model for sustainable, locally-owned family planning and adolescent health programs in the Philippines.
Author: Dr. Anthony Faraon, ZFF TCI-Philippines Chief of Party
Iloilo City Takes Bold Steps in Family Planning and Adolescent Health
Iloilo City has been working hard to improve its Family Planning (FP) and Adolescent Sexual and Reproductive Health (ASRH) services since joining The Challenge Initiative (TCI)-Philippines in May 2023. With committed leaders and policies based on data, the city is making huge progress in bringing health programs closer to communities and solving long-standing problems with high-impact, locally adapted solutions.
A recent trip to the field on August 20, 2025 gave a firsthand look at the progress being made and the energy that everyone is putting into it.
Health in Action in the Community
The opening of Iloilo City’s first PuroKalusugan in the Arevalo District was a big step forward for community-based service delivery. This program provides health services right to the purok, which is the smallest unit of a community. This makes healthcare easier to get, especially for people who don’t have access to it.
At the launch, attendees had access to a full range of services, such as PhilHealth membership, consultations on maternity and child health, family planning counseling and provision, adolescent health services, nutrition support, and vaccinations. Putting services together shows that there is a plan to cover several health requirements in one easy-to-reach place.
I met two young doctors, Earl Sevilla and Lysander Quintia, working as health center physicians in Iloilo. They are examples of what it truly means to serve the public. Even though they didn’t have a lot of resources and were dealing with problems like teenage pregnancy, rising cases of sexually transmitted diseases (STIs), and the growing trend of vaping among young people, Sevilla and Quintia were nevertheless very determined and passionate. Their choice to work in community settings instead of more lucrative jobs shows how strongly they care about public health and equity.
Related articles:
- Iloilo’s Youth Health Movement in Action
- Eight Cities Share Success in Family Planning and Adolescent Health
Leadership That Listens and Leads
Strong leadership is setting Iloilo’s health agenda at the policy level. During a visit to City Hall, Vice Mayor Lady Grace Julie Baronda, a vibrant leader with legislative experience, showed great interest in learning more about the health concerns that need policy assistance or institutionalization. Her willingness to a dialogue shows that she believes in a style of government that values evidence, working together, and community voices.
Grace Hofilena, representative from the Office of Mayor Raisa Trenas, said the same thing. She conveyed that the Mayor strongly supports the program and wants to keep working with TCI. This support from institutions is really important for sustainability and ensuring programs and policies have lasting effect.
The City Leadership Team’s data shows the results of these concerted efforts. From 2020 to 2025, the modern contraceptive prevalence rate (mCPR) went up from 39% to 41%, while the percentage of demand satisfied* rose from 79% to 88%. Although the adolescent birth rate (ABR) has stayed the same at 19 per 1,000, it is evident that further action is needed.
The city’s big budget increase for family planning—from 765,000 pesos in 2023 to 8 million pesos in 2025—may be the best indicator of political will. This jump shows that FP is not only a programming priority, but also a financial one, thanks to excellent leadership.
Persistence and Progress
When local leaders, health workers, and communities work together toward a common goal, like they did in Iloilo City, progress in public health is both attainable and realistic. But there are still challenges. Teenage pregnancies, STIs, and dangerous behaviors among teens are still putting a lot of stress on the system. To solve these problems, we need more than just technical fixes. We need to keep coming up with new ideas, work together across sectors, and get the community involved.
The field visit showed not only what the city has done well, but also the qualities that support those achievements: compassion, resilience, and responsibility. Health workers are making services more accessible to people who live nearby. Local leaders are using policy and budgets to drive sustainability. And young professionals are putting service and making a difference ahead of their own interests.
A Model for Local Health Governance
The last two years have shown how powerful local governments can be in Iloilo City. They can achieve real, quick progress in important health areas when they have the necessary tools, data, and assistance. The city’s increasing investments in FP and ASRH demonstrate that robust political commitment, alongside community-driven innovation, can yield tangible outcomes.
The lessons from Iloilo are clear: to improve family planning and adolescent health, we need more than just one-time action. It needs changes to the whole system, shared accountability, and working together. Iloilo City is a great example for other communities in the Philippines that want to invest in the health and future of their families and young people.
—
* Demand satisfied refers to the percentage of women of reproductive age who want to delay or avoid pregnancy and are actually using a modern contraceptive method.
Author: Dr. Anthony Faraon, ZFF TCI-Philippines Chief of Party
No Detours: Building Expressways to Adolescent Health
The road to a healthier future for Filipino youth is not a scenic route—it’s an expressway we need to build now. Last week in Bohol, at the Adolescent Health Learning Exchange (AdHLEx)—organized by the Department of Health (DOH) Adolescent Health Unit and DOH Center for Health Development VII—government leaders, health professionals, civil society, and young people gathered to map that route.
The metaphor of roads—national highways, boulevards, crossroads, and yes, rough roads—showed both how far we had come and how far we had fallen off the track. On the “national highway” are broad policy frameworks like the Universal Health Care (UHC) Act and the Responsible Parenthood and Reproductive Health (RPRH) Law. On the “boulevards” are adolescent sexual and reproductive health (ASRH) services. At the “crossroads” stand local governments and multi-sectoral teams deciding whether to press forward or stall. Far too many young Filipinos also find themselves on “rough roads” marked by early pregnancy, mental health struggles, and lack of access to care.
National data gives us a mixed view. According to the Commission on Population and Development (CPD), adolescent birth rates (ABR) in the Philippines have generally declined in recent years—a sign that sustained interventions are working. However, there has been a rise in births among girls aged 10 to 14 years old, which is a real concern. These pregnancies are often the product of abuse and exploitation, and they can have lifelong consequences for the health, education, and well-being of these children. This is not just a statistic—it’s a warning sign.
The lesson from Bohol is crystal clear: adolescent health cannot be treated as a side street. It must be central to our public health and development agenda. That means three things.
First, integration. ASRH is not separate from mental health, nutrition, or protection from abuse—they are all part of the same path. A national plan that doesn’t reach the barangay health station or school clinic is a highway that ends in a dead zone.
Second, youth participation. In Bohol, young leaders were not tokens on a panel; they were drivers of solutions—designing peer-led programs, confronting stigma, and reaching peers in ways adults can’t. We cannot plan adolescent health “for them” without planning it “with them”.
Third, scaling innovation. From peer education networks to mobile health clinics, the solutions already exist in pockets of the country. The challenge is not invention—it’s political will, financing, and replication at scale.
This is where the work of The Challenge Initiative (TCI)-Philippines offers important lessons. In 24 cities across the country, TCI has worked with local government units (LGUs) to make high-impact practices for ASRH a permanent part of their work. These include strengthening leadership teams, training health workers, making health facilities more welcoming to young people, and embedding adolescent health in local investment plans.
Related article:
For example, in several LGUs where TCI support was sustained, adolescent birth rates among 15–19-year-olds dropped significantly within a few years. Cities have adopted referral systems linking schools, barangay health stations, and hospitals; improved commodity security for contraceptives; and launched social behavior change campaigns that reach both in-school and out-of-school youth. These are not just pilot initiatives that go away when funding ends—they are built into LGU budgets, policies, and processes.
TCI’s approach proves that with local ownership, data-driven planning, and community engagement, adolescent health programs can produce measurable results. But the rise in pregnancies among the youngest girls shows there are still gaps in protection, prevention, and early intervention. LGUs need to strengthen links with child protection mechanisms, expand mental health services, and equip frontline workers to detect and respond to abuse swiftly.
The Special Health Fund under the UHC Law offers an untapped opportunity. LGUs can earmark these pooled resources for adolescent health—financing outreach programs, peer education, and youth-friendly clinics. Schools can become gateways to care, not just sources of information, by partnering with health providers for on-site services. Communities can become safe spaces where adolescents access help without fear or shame.

We are in a race against time. Every delay means another young life derailed by preventable pregnancy, untreated mental health issues, or violence. The choice is ours: keep patching potholes, or build the expressways our adolescents deserve.
At AdHLEx, we chose the latter. Leaders from national agencies, local governments, and the youth sector committed to accelerate progress, address the alarming rise in pregnancies among the youngest girls, and ensure every adolescent in the Philippines can grow up healthy, educated, and safe.
The rest of the country must follow—not someday, but now.
Author: Dr. Anthony Faraon, ZFF TCI-Philippines Chief of Party
From Momentum to Milestone: Mandaluyong City’s TCI Journey
When Mandaluyong City joined The Challenge Initiative (TCI)-Philippines in 2023, it did so with quiet determination and a clear sense of purpose. Mayor Benjamin Abalos Sr.’s letter of intent wasn’t just a formal document—it was a signal that the city was ready to invest in the future of its people, especially women and young people, by prioritizing access to quality family planning (FP) and adolescent and youth sexual and reproductive health (AYSRH) services.
At the time, Mandaluyong’s modern contraceptive prevalence rate (mCPR) stood at 22%—still far from the national target of 37%. The adolescent birth rate (ABR) was 13 births per 1,000, better than the national average but showing an erratic pattern. These numbers gave us a snapshot: progress, but also room (and reason) to do more.
Through a collaborative Program Design Workshop in November 2023, city stakeholders and the TCI team got to the heart of the matter. Together, three key challenges surfaced: fragmented coordination across departments, widespread myths and misconceptions about FP, and a lack of trained personnel. Familiar challenges, yes—but the way Mandaluyong tackled them was anything but typical.
The city immediately set up a City Leadership Team (CLT), pulling in champions from different departments. This team wasted no time adopting five of TCI’s high-impact practices (HIPs): strengthening health leadership, engaging communities, making services more adolescent-friendly, improving post-pregnancy family planning, and empowering community health volunteers. Each intervention was locally driven and tailored to Mandaluyong’s needs.
Related article:
Since then, it’s been a steady roll-out of smart, strategic, and scalable actions. Health workers have been trained on everything from informed consent to subdermal implants to intrauterine device (IUD) insertion. Youth leaders were engaged through the Sangguniang Kabataan orientation. Population workers, health leaders, and facility staff were brought into the fold through orientations, workshops, and coaching sessions. Alongside that, the city integrated FP and AYSRH programs into local events like the Adolescent Congress, Healthy Buntis Pageant, and Family Planning Month—turning awareness into action.
Fast forward to today: the city has built a solid foundation for long-term self-reliance. There’s now a pool of Master Coaches mentoring others, a trained workforce offering quality FP and AYSRH services, a functional and empowered CLT, and an operational Health Management Information System that helps track performance and identify gaps. Even more affirming, the LGU has continued to increase its local investment in FP and AYSRH—a strong signal of ownership.
The results are real: mCPR has gone up to 23.4%, and ABR has remained stable at 13. These may sound like small shifts, but they represent steady, measurable progress—especially in a field where change doesn’t happen overnight.
And here’s what excites us even more: as of July 2025, there’s been a change in leadership in Mandaluyong. Mayor Carmelita “Menchie” Abalos, previously the Vice Mayor, is now at the helm. It’s clear that continuity is likely—especially with strong advocates like City Health Officer (CHO) Dr. Arnold Abalos and Assistant CHO Dr. Emily Detaro still championing FP and AYSRH from within. Their commitment, paired with Mayor Menchie’s openness to sustain the work already in motion, gives us confidence that the city’s momentum won’t just continue—it’ll grow.
Mandaluyong’s journey with TCI is a solid example of what can happen when cities lead from the front—when political will, technical capacity, and community ownership come together with purpose. We’re looking forward to officially recognizing Mandaluyong as a self-reliant city on FP and AYSRH by September.



